SPOR EA - Cost Accounting for Long-term Care Beds - Project Development - 2/10 - 2025 05 30
The purpose of this work is to make visible the work that is erased from social and health cost accounting, the work of the family caregiver. We are invisible no more.
INTRODUCTION
This article describes the genesis of how this project developed its approach to understand cost accounting for operating long-term care beds in institutional and home-based settings. The article is organized in three sections: 1. Project development for the Scoping Review; 2. Project development for collecting and reporting first-hand cost accounting data from a single home-based caregiving operation (Family Caregiving); and 3. Discussion Notes arising from the presentations.
Our home-based family caregiving operations started approximately six months before I started working on research to understand our lived experience of taking on the life and death responsibility for our frail elder with complex needs.
We have an ethical imperative to improve outcomes for family caregiving households.
1. SCOPING REVIEW
The research topic funded by Strategy for Patient Oriented Research Evidence Alliance (SPOR EA) was, “Cost-effectiveness of home care versus assisted living facilities for individuals requiring additional supports” (funding notification 2023 07 31).
I started discussions about this topic approximately six months after Mom moved home (May 2022).
The idea started as a potential project idea to help other families prepare for the reality I was now living, "Elders In-Home - Planning for Advanced Care". The purpose of this project was to, "... help families plan for Elder in-home caregiving - to understand the health context for providing in-home advanced health care; to utilize public and private support services; to plan for necessary home alterations; and make financial plans to support the transition and continuing caregiving."
I had pulled together a team comprised of a Research Services Lead, Private Home Support Service Provider, Residential Renovation Contractor, Residential Finance Specialist, and myself, a Professional Project Manager and Curriculum Developer.
Our idea was to put together a course offering for Seniors and their family members to talk about aging and how to put plans in place to meet needs when aging family members can no longer fend for themselves. Without funding to support project development, the idea was shelved.
I felt there had to be a place for elders and family members to prepare as the realities of aging and loss of function became a day to day pre-occupation. At the start of my third month of caregiving I entered these notes in my journal:
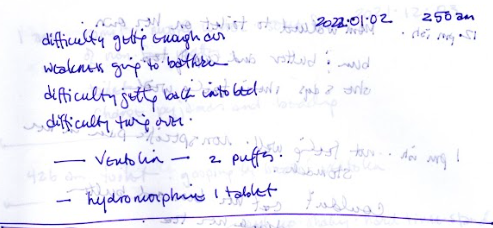 |
| 2022 01 02 - how the day began - 2:50 am |
 |
| 2022 01 02 - how the day ended - 11:35 pm |
On August 31, 2022 I received notification of a call for research topics from SPOR EA. The deadline to submit topic ideas was September 30, 2022.
I consulted with leadership at Family Caregivers of BC and Patient Oriented Research facilitator, as well as attending the first of a six instalment webinar series titled, "Building a Better System to Support Canadian Family Caregivers"
The first session was titled, "Recognizing the Family Caregiver Role".
It was held on SEPTEMBER 20, 2022. 12:00–1:30 PM MST
"Family caregivers have been called the "Invisible Workforce" and the "Backbone of the Healthcare System," yet family caregivers are not recognized in policy nor as partners in care by health and social care providers. The lack of recognition of the family caregiver role was particularly evident during the COVID-19 pandemic, as family caregivers were referred to as 'visitors.' This conversation aims to answer the question, "How do we improve recognition of family caregivers and the importance of the family caregiver role?""
I kept hearing about the unaccounted cost of family caregiving, which I was enduring first-hand.
 |
Eales, J., Fast, J. E., Duncan, K., & Keating, N. C. (2022, February 20). Family Caregiving Worth 97 billion.pdf. University of Alberta, Department of Human Ecology.
|
2. FAMILY CAREGIVING (Case Study of One)
When Mom moved home she was extremely frail and weak from undiagnosed pneumonia, an exacerbation of her end-stage Chronic Obsrtuctive Pulmonary Disease (COPD). When she moved home she was still smoking cigarettes, a forty-year habit. During those first few weeks, Mom had difficulty breathing. We put her on antibiotics and various ventilating puffers to help her get enough air. There at least two moments when I didn't know if she had taken her last breath and I didn't know what to do. Did I call my siblings and alert them of Mom's dire situation? Did I sit quietly with Mom and keep her as comfortable as I could? Mom was adamant that she did not want to go to the hospital. If this was her last breath, she was clear that she wanted to, "Let nature take its course." I understood the mission, I accepted the mission, I had never done anything like this before.
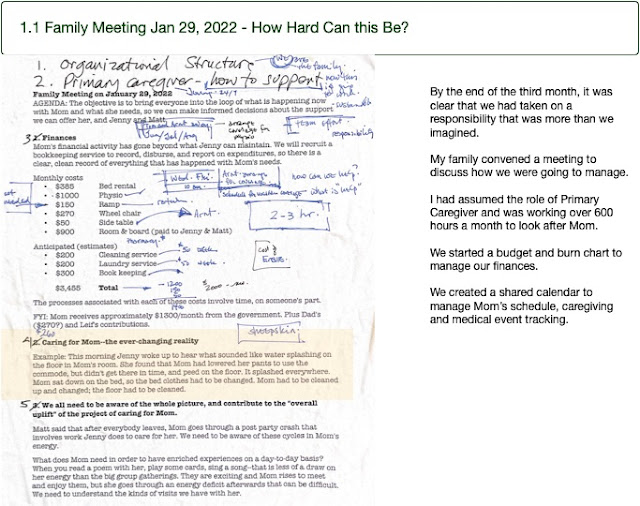
The first six months I was providing unpaid care for Mom over 600 hours a month, as well as trying to maintain my paid consulting work as a full-time project manager. We signed all the papers for Expected Death in the Home, Do Not Resuscitate Order, and Mom was put on the Palliative Care Registry for a six month period. I was determined to keep Mom home, I was operating in crisis mode, thinking that I could handle whatever was coming for the next six months.
Mom's registration for home-based Palliative Care included services for her personal care (bathing) and respite (2 hours a week). The service was very specific that it was only for Mom's personal needs, there was no provision for the caregivers to do any housework or cooking (what I understood). I felt pressure to ensure everything was in good order when a caregiver came to give Mom her bath, I didn't want to be seen as neglecting Mom's needs for a clean, orderly household.
On January 29, 2022, my family held a meeting to review where we were with Mom's care and how we were going to manage going forward.
We started working with planning documents to manage time, finances and Mom's health needs. As of February 1 we had started using a shared Google Drive, including Google Calendar, to track Mom's day to day, week to week schedule and caregiving needs.
This Google calendar became my data source for time records. I used it to calculate the amount of time I was on duty looking after Mom, also the amount of time other family was contributing, and finally the impact of Home Support Respite and also paid caregiving from a private contractor. The Google calendar also gave me a fairly accurate portrayal of the daily tasks and visits entailed in looking after Mom.
I kept rigorous financial data records because I had Power of Attorney over Mom's finances. I was scrupulous to ensure every transaction in and out of her bank account was traceable. I had the same level of detail to track funds related to Mom's care that passed through my bank account. I had first-hand financial records for all costs associated with the property.Link to Family Caregiving Cost Accounting Presentation slides
3. DISCUSSION NOTES
Were costs reported in the Scoping Review - did they cover costs for Medical Doctor, Registered Nurse or Home Care Worker? We did not have that information available from the study.
Is there data available that measures how much time / care are being contributed by families in institutional settings? There was one study that reported this amount of time was estimated to be 40 hours a month.
What are the differences between in-home long-term care and home care services? Home care services would be a sub-set of services provided to support in-home long-term care.
How was time quantified to a dollar amount? What rate was applied for the time? This was variable depending on the level of professionalism of the caregiver.
We are trying to compare the cost of providing formal care in the home-based setting and the cost of informal (family provided) care.
Did the caregiving time cost reported for Family Caregiving include all levels of function to run the operation? Yes, that time was included in the lump sum amount of time.
How do you value the time of a home-based family caregiver in relation to the time cost of an institutional setting? We don't have a breakdown to compare the time cost per patient per bed between an institutional and a home-based setting.
A question about methodology - how was the consideration for cost of living factored into the per day cost for home-based caregiving? We factored cost of living based on square footage as if the space was reporting expenses according to tax requirements.
If the family had given up providing long-term care for our Mom, the cost of that caregiving bed would have been transferred to the healthcare system. We need to have a social, a society conversation about who has the responsibility to care? Who should be responsible, and how should the cost of care be shared? Who supports the people who take the responsibility for caring?
There is a similarity between the costs and work incurred by families looking after medically complex kids, we can use this work to help understand and support those caregiving operations, too.
How do we think about quality and risk management in a home-based caregiving setting? Can we look at how quality and risk management are implemented in an institutional setting and see what can be generalized across all caregiving beds?
2022 11 22 Mom singing, "Long, Long Ago" for her granddaughter on a visit a year after she moved home and a year after she was put on the Palliative Care Registry.CONCLUSION
=========================================================================
SPOR EA - Cost Accounting for Long-term Care Beds
funded by Strategic Patient Oriented Research (SPOR) Evidence Alliance
Table of Contents
Introductory - Follow up / Thank You - 0/10












Comments
Post a Comment